When you’re expecting a baby, there is no greater priority than making sure you and your little one are safe. For most parents, the idea of something going wrong is unsettling. Unfortunately, complications during pregnancy and delivery can happen—including serious conditions like placental abruption.
Placental abruption is a potentially life-threatening condition that can lead to serious birth injuries, devastating families in an instant. If medical negligence played a role, you deserve answers and may have legal options to seek justice and compensation.
What Is Placental Abruption?
Placental abruption occurs when the placenta, the organ that provides oxygen and nutrients to the baby, prematurely separates from the wall of the uterus before delivery. It is a is a serious obstetric emergency that endangers both mother and fetus. It occurs in approximately 0.6–1.2% of pregnancies in the United States, with nearly half occurring in term pregnancies. Yet, placental abruption can disrupt the baby’s blood and oxygen supply and can lead to severe complications for both mother and child, depending on the degree of detachment.
Types of Placental Abruption
Placental abruption can also be classified by severity: it may be partial (separating marginally or in part) or complete, and bleeding can be visible or concealed (hidden behind the placenta).
- Partial abruption: Only part of the placenta detaches, and symptoms may vary in severity.
- Complete abruption: The entire placenta detaches from the uterus, which is a medical emergency requiring immediate intervention.
Symptoms of Placental Abruption
Diagnosing placental abruption is challenging and is largely based on clinical presentation. Signs of placental abruption can develop suddenly and may include:
- Vaginal bleeding (which can range from obvious and heavy to minimal or absent if bleeding is concealed)
- Severe abdominal or uterine pain (often sudden and severe in the case of abruption, unlike the painless bleeding of placenta previa)
- Uterine tenderness or rigidity
- Reduced fetal movement
- Contractions or preterm labor (the uterus may contract excessively due to the irritation of blood)
If these symptoms arise, seeking emergency medical care is critical. Swift action is essential for protecting the health of both the mother and the baby.
It’s worth noting that not all abruptions present with visible bleeding. In a concealed abruption, blood collects behind the placenta and the classic symptom is intense pain with a rigid uterus and shock/disseminated intravascular coagulation out of proportion to external blood loss. Because of this variability, clinicians maintain a high index of suspicion for abruption in any case of unexplained uterine pain or tenderness in late pregnancy.
Imaging studies like ultrasound can be used to help evaluate suspected abruption. For example, ultrasonography may show a clot (hematoma) behind the placenta or other abnormalities. But importantly, a normal ultrasound does not rule out a placental abruption. The diagnosis is primarily clinical, made by correlating the patient’s symptoms and exam with exclusion of other causes.
Potential Consequences of Placental Abruption
Placental abruption can have moderate to severe impacts, depending on the extent of the separation and how quickly medical professionals respond.
Risks to the Baby
The fetus is directly endangered by placental abruption because the placenta is the baby’s lifeline for oxygen and nutrients. When a significant portion of the placenta separates, the baby can become deprived of oxygen (a condition known as uteroplacental insufficiency or acute asphyxia). The outcomes for the baby depend on the extent of separation and how quickly the baby can be delivered (as well as the gestational age). For the baby, a lack of oxygen and nutrients caused by placental abruption can lead to:
- Brain injuries: Conditions like hypoxic-ischemic encephalopathy (HIE) caused by oxygen deprivation can result in long-term developmental delays or cerebral palsy. The interruption of blood flow from a placental abruption can cause acute oxygen deprivation in the fetus. Surviving infants often show signs of hypoxic-ischemic encephalopathy (HIE), which is brain dysfunction caused by lack of oxygen/blood during birth. One large review found that placental abruption is associated with a greatly increased risk of neonatal encephalopathy: 17% of infants diagnosed with moderate/severe HIE had evidence of an abruption, compared to around 1% incidence of abruption in the general birth population. In another study, 29% of babies either suffered HIE or died.
- Preterm birth: Placental abruption is a leading cause of premature delivery, which carries additional risks such as breathing issues or feeding difficulties.
- Stillbirth: Complete placental abruption significantly increases the risk of a pregnancy ending in loss.
In summary, placental abruption is very dangerous for the baby. Without the placenta, the fetus cannot survive; thus, a significant abruption can kill or permanently injure the baby. Many will require NICU care, and some may have long-term neurodevelopmental impairments (e.g. cerebral palsy, cognitive delays). Swift recognition and intervention are crucial to prevent these outcomes.
Risks to the Mother
The mother may also face serious complications, including:
- Extensive blood loss: Abruption can cause torrential bleeding (sometimes overt, sometimes concealed), leading to hypovolemic shock. The mother may require urgent blood transfusions to stabilize. Severe hemorrhage can also necessitate procedures up to an emergency hysterectomy if uterine bleeding cannot be controlled
- Organ damage, such as kidney failure from severe hemorrhaging risk of complications in future pregnancies
- Emotional trauma from a traumatic delivery or loss of the baby
In summary, placental abruption is a life-threatening event for mothers due to hemorrhage and its effects. The obstetrical team must be prepared to manage massive bleeding (with IV fluids, blood products, and possibly surgical intervention) and monitor/treat coagulopathy. Maternal intensive care unit (ICU) admission is common in severe cases. With proper and rapid care, most mothers survive.
The Role of Medical Negligence
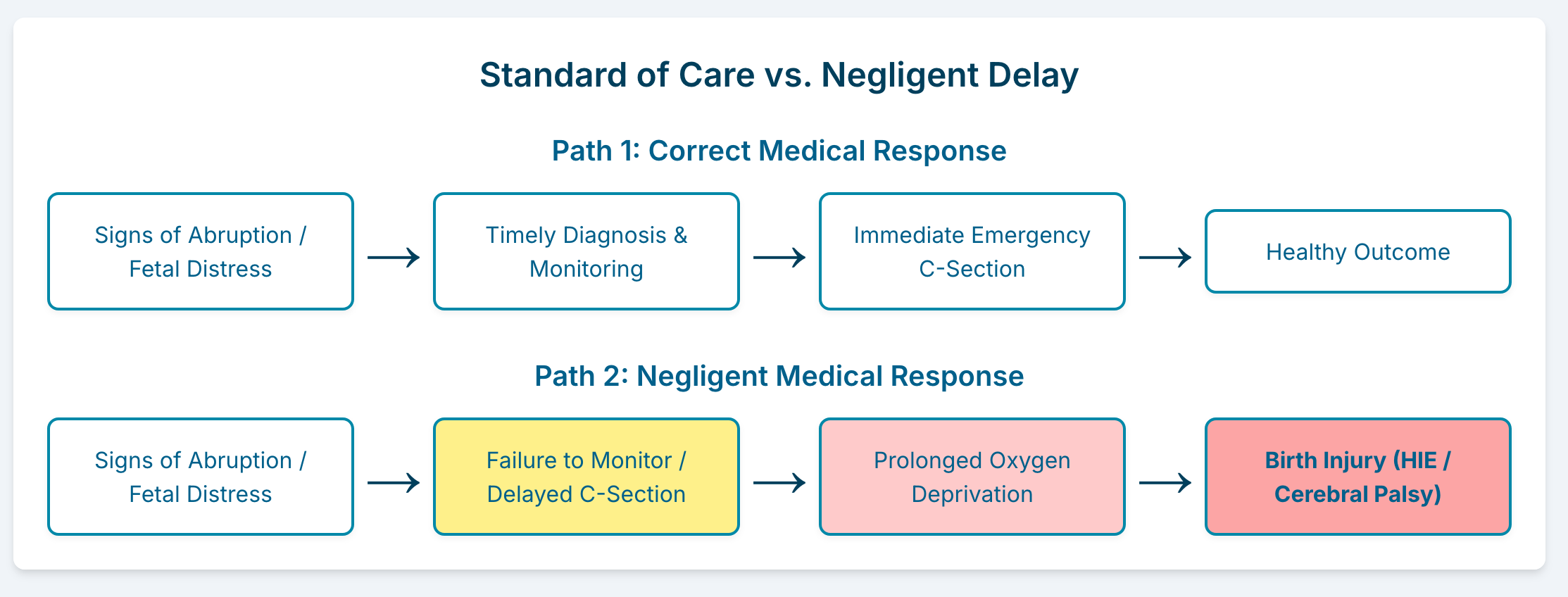
In obstetrics, the adage “time is of the essence” applies to placental abruption. Every minute of separation increases the risk of fetal brain damage or death and worsens maternal hemorrhage. Medical negligence can significantly worsen the outcomes of placental abruption. Doctors and medical staff play a critical role in monitoring pregnancy for warning signs and responding promptly when complications arise.
Providers must deliver the baby and placenta as soon as safely possible to stop placental bleeding and rescue the fetus from an oxygen-deprived environment. In many cases, this means an emergency cesarean section. According to studies, “in the presence of fetal or maternal compromise, prompt delivery by cesarean is often indicated.”
Further, prompt maternal stabilization is needed with large-bore IV access, fluid and blood transfusions, and an experienced obstetric and anesthesiology team. Blood products like plasma and cryoprecipitate may be needed also. A massive transfusion protocol and critical care specialist involvement are often activated in abruption cases.
In summary, managing placental abruption requires timely action. Signs of instability prompt urgent delivery to prevent severe outcomes because prolonged abruption with ongoing separation increases the risk of fetal hypoxia.
When Placental Abruption Goes Unnoticed
Medical care quality and timeliness are crucial for mother and baby outcomes after an abruption occurs (or risk factors emerge). In medical negligence or malpractice, key issues include failing to promptly recognize and manage placental abruption or its leading conditions. If medical professionals fail to identify or act on symptoms of placental abruption in time, the consequences can be devastating. Examples of medical negligence include:
- Ignoring warning signs such as maternal bleeding or pain. Delaying placental abruption diagnosis can be catastrophic. Prompt action is crucial to prevent prolonged oxygen deprivation to the fetus. Fetal monitoring and timely ultrasounds are essential to differentiate from placenta previa. Misinterpreting symptoms, such as vaginal bleeding, can delay diagnosis. Clinical vigilance is critical: One study emphasizes that accurate assessment is “accurate patient assessment is critical to developing an appropriate management plan and preventing a potentially poor outcome.”
- Failing to monitor the baby’s oxygen levels or heart rate during labor. Placental abruption can evolve, with small marginal abruptions worsening over hours. Sending a patient home with concerning symptoms is risky. Instead, providers should observe significant vaginal bleeding or abdominal trauma to prevent a delayed abruption. Failing to do so could miss an opportunity to intervene early. Similarly, after stabilization, monitoring maternal vital signs and fetal heart rate is crucial to prevent a catastrophe from progressing unnoticed. “Continuous electronic fetal monitoring is initiated to identify prolonged bradycardia, decreased variability, and the presence of late decelerations.” These are all non-reassuring signs for the baby that require providers to promptly intervene.
- Delaying critical interventions like a C-section. Once an abruption is recognized (or even strongly suspected), the standard of care is to respond quickly and skillfully. This includes mobilizing resources for an urgent delivery and maternal stabilization. If there is any failure in the response – for example, a delay in performing the C-section, not having blood on hand for transfusion, or lack of proper monitoring – the results can be dire. Obstetric teams are trained for these scenarios, and most hospitals have protocols. Not following protocol can be negligence. ACOG and obstetric consensus stress the importance of a coordinated team for abruption management.
- Mistakes during prenatal care that increase the risk of abruption, such as mismanagement of conditions like high blood pressure or diabetes
In conclusion, medical negligence in placental abruption cases typically relates to delays or failures in recognition and response. The medical literature makes clear that rapid, well-coordinated management is essential to improve outcomes in abruption. When these lapses in care occur, the healthcare provider may be held legally responsible for the harm caused to both the mother and baby. Conversely, when managed appropriately, some of the worst outcomes (like hypoxic brain injury) may be mitigated.
Legal Options for Families Affected by Placental Abruption
If your family has experienced a birth injury related to placental abruption, you may feel overwhelmed. Understandably, your top priority is caring for your child and recovering from the experience. However, holding negligent parties accountable can provide financial support and prevent similar incidents in the future.
What Compensation Covers
Through a medical malpractice claim, families may be entitled to compensation for damages such as:
- Medical expenses for the mother and baby, including long-term therapy, medical and attendant care needs
- Lost wages if parents must miss work to care for their child
- Pain and suffering caused by the trauma of the injury and its aftermath
- Additional costs, such as modifications to your home for a child with special needs
Steps to Take
Legal cases of placental abruption are scrutinized to ensure no preventable delays or mismanagement occurred. Experts investigating birth injuries related to abruption ask if providers acted with the urgency and competence required for this critical condition. If not, it could indicate medical negligence contributing to the harm.
To protect your legal rights, take the following steps:
- While in the hospital: document and record everything. Many people have a notes app on their phone. (Old fashioned pen and paper also work but make sure you save it.) When providers check in with you, note the time and what they did or told you. This will help you remember the sequence of events afterwards.
- Request medical records. Documentation of your prenatal care, delivery, and post-birth treatment is vital evidence for evaluating potential negligence.
- Consult a birth injury attorney. A legal professional can help you understand whether negligence played a role and guide you through the legal process.
- Act quickly. Medical malpractice claims are subject to time limits or statutes of limitations, which vary by state. Consulting an attorney promptly can ensure you don’t miss your window to file a claim.
Birth Injury Attorneys
Placental abruption is a significant concern with implications spanning medical, legal, and emotional domains. With your journey through understanding this complex condition, consider reaching out to National Trial Law, where comprehensive legal support is available for families navigating the aftermath of birth injuries. Our team is dedicated to advocating for your rights and providing the expertise needed to address the complexities of medical malpractice claims. Reach out today at (833) 913-1885 to learn how we can support you through these critical times. Empower your journey with the right legal partner by your side.

